Skyland Trail is a trailblazer in the area of measurement-based care and outcomes research, which is an integral part of our evidence-based treatment model. Our robust outcomes and research program employs evaluative instruments considered to be the gold standards in the mental health field to measure the effectiveness of our treatment programs.
Outcome data from 2008 through 2020 confirm that our unique integrated, evidence-based approach helps our clients return to their communities with reduced symptoms and improved skills to pursue more independent and productive lives.
2020 AREA OF FOCUS
In 2020, we explored the impact of childhood trauma on treatment outcomes.
Prefer to View a PDF?
View or print a PDF of the 2020 Outcomes Report
2020 ADULT OUTCOMES RESEARCH REPORT
2020 Client Community
Age at Admission
Gender
Primary Diagnosis at Discharge
Adult Patient Complexity
Skyland Trail has specialized in treating complex patients for many years. Many patients enroll in the residential treatment program after participating in other outpatient or inpatient therapeutic programs without results.
In 2020, Skyland Trail treated a large number of young adult patients ages 18 to 25 with a complex constellation of co-occurring disorders: a mood disorder, borderline personality disorder, and a substance misuse disorder. Patients in this category had outcomes similar to the broader patient population and experienced significant improvement in symptoms, functionality, and hopeful thinking.
61% of clients
had >3 co-occurring diagnoses confirmed at discharge
Co-occurring disorders include: anxiety disorders, substance misuse, borderline personality disorder, others
2020 Adult Programs Key Outcomes
Improved Functioning
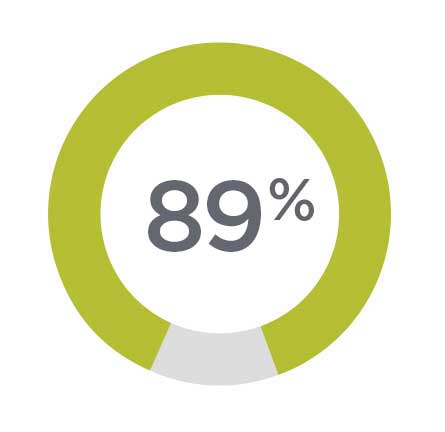
89% of all patients
experienced a clinically significant improvement in functionality, symptoms and social relationships 1

Improved Hope
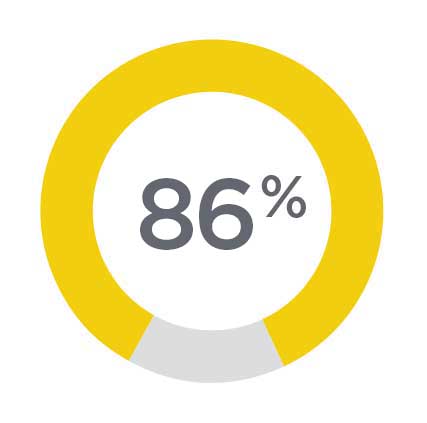
86% of all patients experienced a clinically significant improvement in hope 2

Improved Medication Attitudes
90% of patients leave treatment with a positive attitude about taking psychiatric medication 3
Reduced Psychosis
86% of patients with psychosis experienced clinically significant improvement in their symptoms of psychosis 4
Reduced Depression
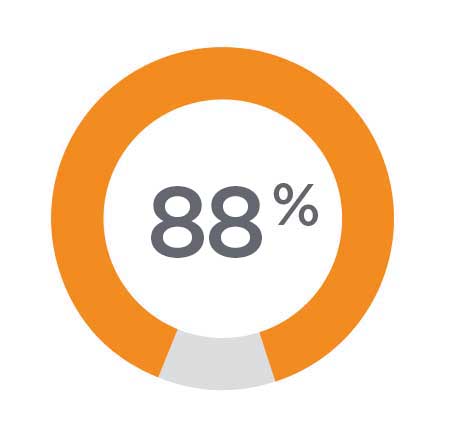
88% of patients with very severe and severe symptoms of depression experienced clinically significant reduction in symptoms 5
Reduced Mania
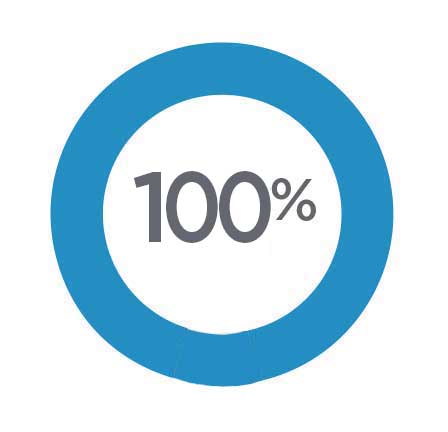
100% of patients who had clinically meaningful episodes of mania showed no symptoms of clinically meaningful mania at discharge 6
(1) The 32-item Behavior and Symptom Identification Scale (BASIS-32): ©McLean University, Affiliate of Harvard Medical School. (2) Beck Hopelessness Scale: Beck AT, Weissman A, Lester D, Trexler L. (1074). The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology, 42(6), 861-865. (3) Medication Attitude Inventory: Hogan TP, Awad AG, & Eastwood R. (1983). A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychological Medicine, 13, 177-183. (4) Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports. 1962; 10:799-812. (5) Montgomery, S.A. & Åsberg, M. (1979). A new depression scale designed to be sensitive to change. British Journal of Psychiatry, 134, 382-389. (6) Young RC, Biggs JT, Ziegler VE, Meyer DA: A rating scale for mania: reliability, validity and sensitivity. British Journal of Psychiatry, 133:429-435, 1978. (7) Hamilton M: The assessment of anxiety states by rating. British Journal of Medical Psychology, 32:50-55,1959.
Adult Symptom Reduction
Skyland Trail administers disease-specific outcome measurement tools every two weeks of treatment, based on the confirmed diagnosis at admission. Though the scales differ for each measurement, lower scores always indicate improved symptomatology.
WORKING TOWARD REMISSION
Historically, when we treat patients with bipolar mania, they are uniformly in remission from mania at discharge, meaning they no longer experience symptoms of mania.
We are looking at how to bring about remission for other diagnoses, specifically depression, and are moving the needle in that direction.
In 2020:
- 31% of clients with major depression were considered in remission - completely symptom free - at discharge
- 40% of patients with major depression improved by 50% or more
- 88% of all patients with major depression experienced a clinical improvement in symptoms
(Based on a comparison of scores on the Montgomery-Asberg Depression Rating Scale at admission and discharge.)
31% of clients with major depression
were considered in remission
at discharge
MAJOR DEPRESSION
88% of patients with very severe and severe symptoms of depression experienced clinically significant reduction
t(222) = 10.30, p =.000
Montgomery, S.A. & Åsberg, M. (1979). A new depression scale designed to be sensitive to change. British Journal of Psychiatry, 134, 382-389.
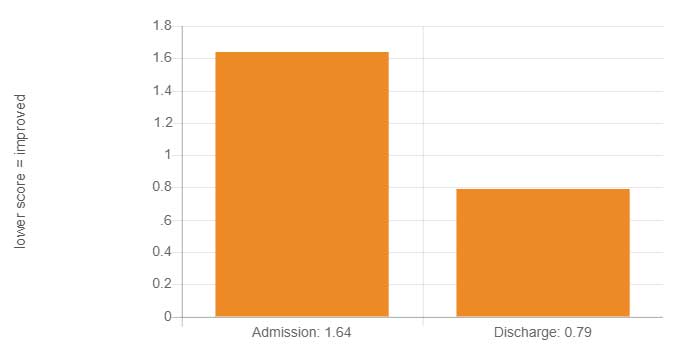
Montgomery-Asberg Depression Rating Scale 2020
BIPOLAR ILLNESS
100% of patients who had clinically meaningful episodes of mania showed no symptoms of clinically meaningful mania at discharge
t(25)= 4.42, p=0.001
Young, et. Al. (1978). A rating scale for mania: reliability, validity, and sensitivity. British Journal of Psychiatry, 133, 429-435.
Young Mania Rating Scale 2020
ANXIETY DISORDERS
85% of patients with anxiety experience clinically significant improvement in control of anxiety
t(202)= 6.44 p=0.000
Hamilton M: The assessment of anxiety states by rating. British Journal of Medical Psychology 32:50-55,1959.
Hamilton Scale of Anxiety 2020
THOUGHT DISORDERS
85% of patients with psychosis experienced statistically significant improvement in their symptoms of psychosis
t(46)= 11.8, p=0.000
Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports. 1962; 10:799-812.
Brief Psychotic Rating Scale 2020
All Adult Client Assessments
These assessments are administered to clients with all diagnoses at admission and at discharge.
IMPROVED FUNCTIONING
In 2020, patients consistently showed statistically significant functional improvement as measured by the BASIS-32. Comprised of 5 subscales, the BASIS-32 contains an overall average score ranging from 0 to 4, with lower scores indicating greater levels of functioning in daily life, interpersonal relationships, impulsivity, psychosis, depression, and anxiety.
Clients as a group showed significant impairment at admission, and low-moderate impairment (and in many cases, no impairment) at discharge.
The 32-Item Behavior and Symptom Identification Scale (BASIS-32). © Copyright McLean University, Affiliate of Harvard Medical School.
Significant Impairment
>1.5 Significant and systemic impairment in daily life and/or interpersonal relationships, with extreme impulsivity, psychosis, depression, and/or anxiety present.
Moderate Impairment
.5–1.5 Moderate impairment in daily life and/or interpersonal relationships, with some impulsivity, psychosis, depression, and/or anxiety present.
Full Functioning
<0.5 Indicates full functioning with no significant impairment in daily life and/or interpersonal relationships, with little or no impulsivity, psychosis, depression, and/or anxiety present.
BASIS-32 Overall Change Scores 2020
t(259)=1302, p<.001
BASIS-32 Subscales Change Scores 2020
Relation to Self/Others
t(259)=1302, p<.001
BASIS-32 Subscales Change Scores 2019
Depression/Anxiety
t(259)=1302, p<.001
BASIS-32 Subscales Change Scores 2020
Daily Living Skills
t(259)=1302, p<.001
BASIS-32 Subscales Change Scores 2020
Impulsivity
t(259)=1302, p<.001
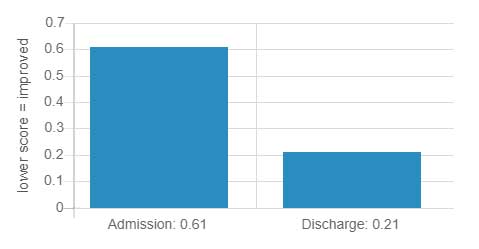
INCREASED HOPEFUL THINKING
In 2020, clients continued to experience a statistically significant decrease in feelings of hopelessness, t(255) = 9.04, p<.001. This finding indicates that, on average, individuals improved from feeling very hopeless at admission to having hopeful future expectations at discharge. Hope for one’s future is one of the best predictors of continued adherence to a recovery plan and protective against suicide.
Human beings are much more than constellations of symptoms, thoughts and behaviors. Hopefulness, social interconnectivity, and a sense of self efficacy define recovery and what it means to be mentally well.
Beck AT, Weissman A, Lester D, Trexler L. (1974). The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology, 42(6), 861-865
Nihilistic Preoccupations
>8 These individuals see very little hope in all domains of their lives.
Some Hopelessness
3–8 Individuals display some hopelessness in their thinking. Individuals closer to 8 can be said to be very hopeless while those scoring closer to 3 can be said to be somewhat hopeless.
Hopeful
<3 Individuals are said to be hopeful.
Beck Hopelessness Scale Scores 2020
t(255)=9.04 p<.001
IMPROVED MEDICATION ADHERENCE
Attitude toward taking psychiatric medications is a surrogate measure for medication adherence. Medication adherence is one of the best predictors of sustained recovery.
Scores on the Medication Attitude Inventory (MAI) range from -10 to +10, with higher scores indicating more positive attitudes towards medication use and medication adherence. On average, clients in 2019 experienced very highly statistically significant improvement with an average attitude score of 4.47 at admission to a 7.10 at discharge.
Hogan TP, Awad AG, & Eastwood R. (1983). A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychological Medicine, 13, 177–183.
>5 Indicates generally positive attitudes towards medication use and are correlated with greater levels of medication adherence in a clinical setting.
Medication Attitude Inventory 2020
t(244)=-11.41, p=.001
IMPROVED ABILITY TO MAKE DECISIONS
A sample of 258 clients who completed the Making Decisions Scale at admission and discharge demonstrated statistically significant improvement in their ability to use self-esteem, optimism, and personal power in making decisions.
A four-point scale, where scores centered around 1 indicate negative beliefs about the ability to make decisions with psychological components like:
• self-esteem
• optimism
• activism
• personal power (beliefs in the efficacy to make decisions on one’s own)
Rogers et al. (1997). A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatric Services, 48(8), 1042-1047.
Making Decisions Scale 2020
SELF-ESTEEM
t(257)=10.16, p<.001
OPTIMISM
t(257)=8.01, p<.001
ACTIVISM
t(257)=8.01, p<.001
PERSONAL POWER
t(257)=6.61, p<.001
2020 Highlight: Childhood Trauma
Trauma exposure has been reported to be associated with inflammatory responses, as has obesity. In 2020, we assessed exposure to childhood trauma through the Childhood Trauma Questionnaire (CTQ) and measured levels of C-Reactive protein (CRP) through laboratory bloodwork in adult clients at admission. We divided a sample of 280 cases with valid CTQs and CRPs into low, moderate, and high cohorts.
- Elevated CRPs were associated with treatment resistance
- Very high elevations (10 or more) in CRP levels were associated with trauma exposure. These elevations were specific to the experience of sexual abuse and were not explained by elevations in BMI.
- There were no linear correlations: sexual abuse was specifically associated with very high CRP.
- The specific experience of sexual abuse leads to an inflammatory response.
Childhood Trauma Rates 2020
(Adults)
As measured by the Childhood Trauma Questionnaire (CTQ) assessment given at admission
Categories of Childhood Trauma 2020
(Adults)
As measured by the Childhood Trauma Questionnaire (CTQ) assessment given at admission
CRP and Specific Trauma Exposure 2020
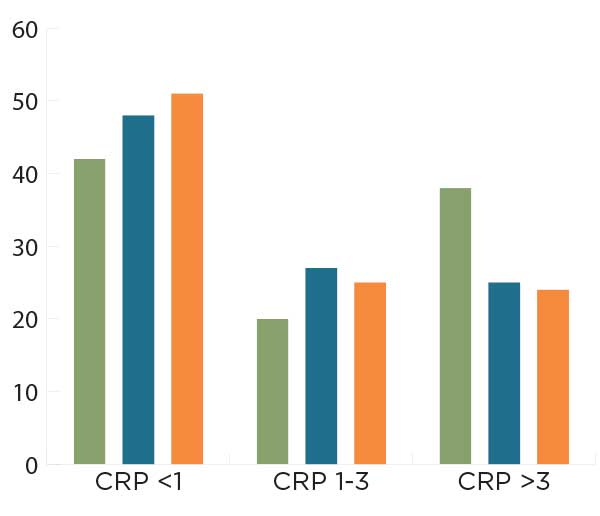
Applications for Treatment
Our goal with this study was to explore a set of predictors to better identify patients who may be at higher risk of treatment resistance or poorer treatment outcomes. If predictors could be identified - for example a combination of CTQ scores and CRP levels - they could be used to target groups of patients early in the course of treatment with specialized interventions to help improve treatment outcomes.
Weight Gain in Treatment
The Wellness Program is working. In 2020, 72 percent of adult clients had no BMI gain. Improvements may be due, in part, to changes in availability of unhealthy meals and snacks due to restrictions imposed for Covid-19 (e.g. fewer off-campus shopping trips, fewer trips to off-campus restaurants, and fewer deliveries of food from visitors) .
72% of adult clients had no BMI gain while in treatment
